Singapore is developing a national action plan to address the increasing resistance of some bacteria to antibiotics.
It is even more of the Singaporeans exposed to such drugs as a quick fix for their disease.
The Ministry of Health (MOH) told the Straits Times that it is working with the Agri-Food and Veterinary Authority (AVA), the National Environment Agency and the National University of Singapore (NUS) to develop a national strategy for antibiotic resistance in Singapore.
This may include educating the public on which diseases should or should not be treated with antibiotics, and on monitoring their use.
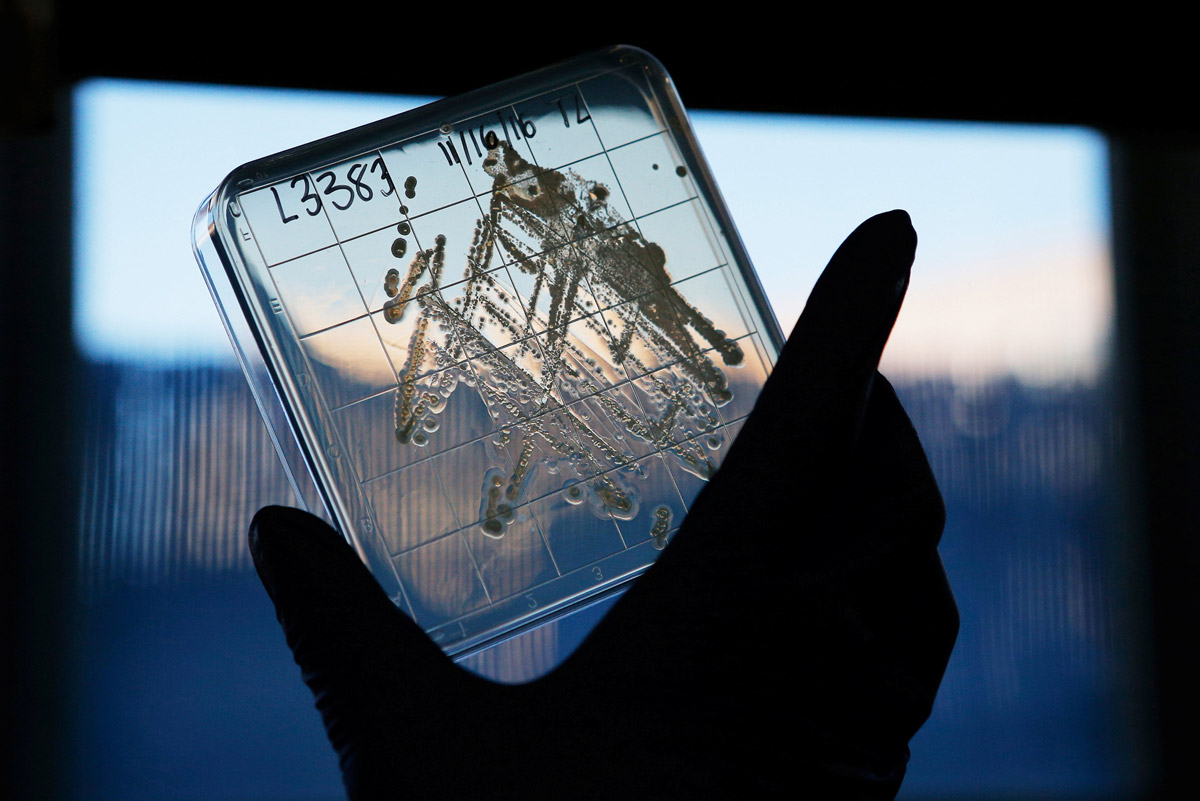
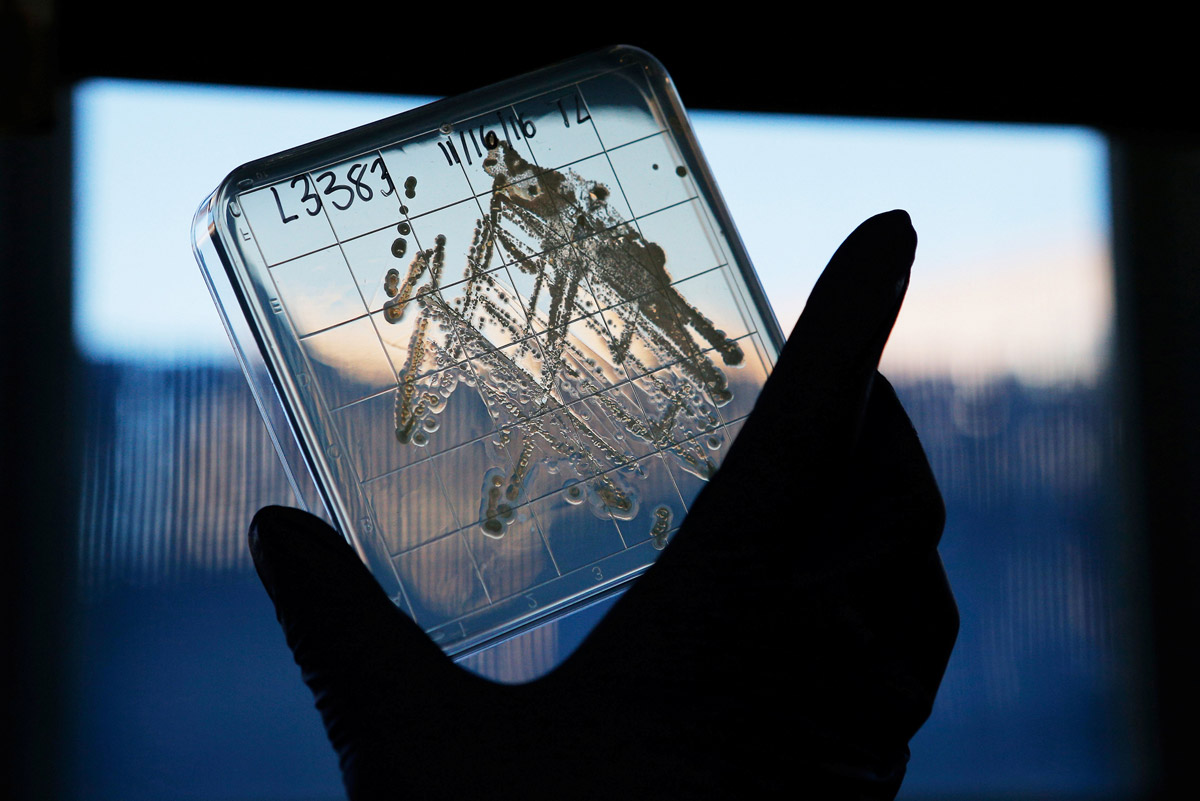
Antimicrobial resistance refers to the ability of microorganisms, such as bacteria and viruses, to resist the effects of drugs that previously could kill them.
When these microorganisms are overused or abused, they are resistant to antimicrobial drugs.
“We are addicted to antibiotics – it has become an integral part of human medicine and livestock industries,” said Dr. Xu Liyang, associate professor and project leader of the Saw Swee Hock School of Public Health ‘s antibiotic resistance program at the National University of Singapore.
The more antibiotics a person takes, the more pressure the bacteria will evolve and become resistant, he adds.
Although the ministry has not provided details of the plan of action, the Straits Times has learned that it may closely follow the World Health Organization’s proposal to address antibiotic resistance.
In addition to targeting human drugs, it is recommended to focus on the use of antibiotics in livestock.
This may mean checking the use of antibiotics in Singapore farms.
AVA currently has a monitoring program for the testing of antibiotic residues in local agricultural products to ensure food safety.
Infectious disease expert Paul Tambyah says there is a need for a holistic approach.
“Public education can help, especially for those who may not need antibiotics, but the reality is that the use of antibiotics in agriculture than human clinics and hospitals to be much more.
Bacteria that have become resistant to antibiotics, including those found in domestic animals, can transfer their resistance genes to other people in the intestine after consumption of meat, especially if they are not properly cooked.
As for human medicine, Dr Tambyah says there is a need for better ways to diagnose the disease so that doctors can target people who actually need antibiotics.
The Ministry of Health currently has guidelines for doctors prescribing antibiotics.
But they are not mandatory.
“This is because not all cases are clear,” says general practitioner Leong Choon Kit.
Even so, doctors generally insist on them, said the interviewer. Dr. Winston Ho, medical director of Parkway Shenton, said that after careful assessment of a patient’s history and symptoms in a specific infection treatment, he decided to prescribe antibiotics.
Patient education is key, he said.
“We are experiencing some patient stress and always prescribing antibiotics for upper respiratory tract infections (URTIs) … They need to know that most acute URTIs are viral and that antibiotics can not be used for viruses.
Investment analyst Issac Foo, 27 years old, said he every time suffering from tonsillitis require doctors to give antibiotics. “My tonsillitis is very serious, unless I take antibiotics, otherwise I will not get better.”
The emergence of deadly super-bacteria makes even the strongest antibiotics invalid also caused widespread concern around the world.
In September, world leaders agreed at the United Nations General Assembly to develop action plans to curb the growing problem of antibiotic resistance.
It was only the fourth time in the history of the United Nations that the General Assembly had discussed a health issue, including the Ebola virus.

This article was first published on Dec 27, 2016.
Get a copy of The Straits Times or go to straitstimes.com for more stories.