SINGAPORE: The surge in dengue cases is due to a “confluence of factors” such as low immunity to certain serotypes of the virus, said the National Environment Agency (NEA) on Wednesday (Aug 5) as the number of cases hit a record high.
A total of 22,403 dengue cases have been reported so far this year, surpassing the annual high of 22,170 in 2013. Twenty people have died from dengue this year as of Aug 2.
Even though the weekly number of cases fell from a high of 1,792 in the third week of July to 1,380 last week, NEA said the weekly numbers remain “persistently high” at above 1,000.
READ: Singapore’s dengue cases reach a record 22,403, surpassing 2013 high
Apart from low herd immunity, the fact that people continue to work from home and an expected high mosquito population in the warmer months of the year mean that Singapore continues to be at high risk for dengue.
LOW HERD IMMUNITY
Singapore’s population has low herd immunity against dengue due to some success in controlling the Aedes mosquito population over the years.
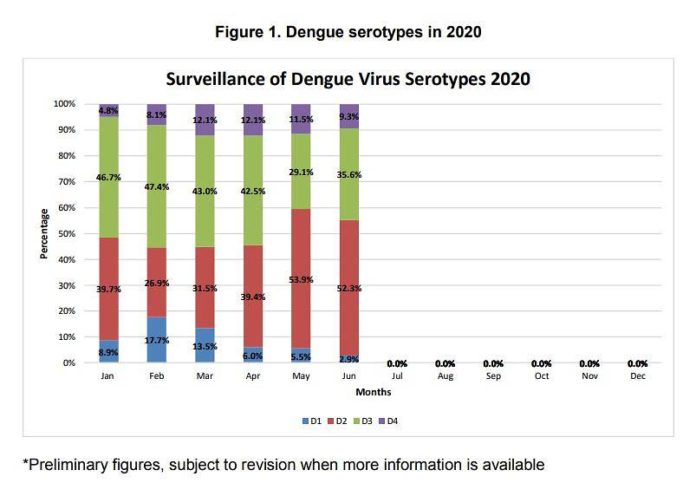
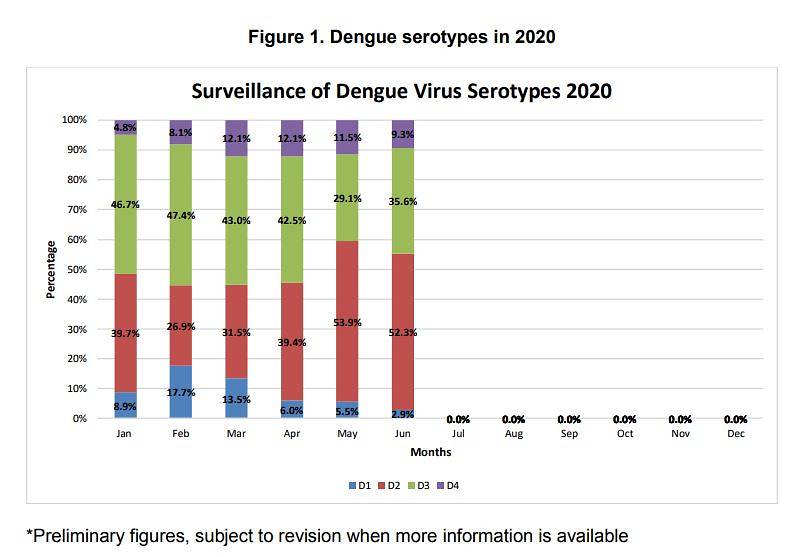
There are four related dengue viruses (DENV-1 to DENV-4) and infection provides immunity against only one serotype. The majority of the infections this year are of DENV-2 and DENV-3.
DENV-2 has been the dominant strain circulating in Singapore since 2016, said Associate Professor Luo Dahai from Nanyang Technological University’s Lee Kong Chian School of Medicine. From last year, there has been a shift of circulating serotype from DENV-2 to DENV-3, he added.
The level of exposure to dengue among young adults here is relatively low, according to the latest study by NEA, published in 2015.
While about 87 per cent of those aged 56 to 60 in the NEA study had immunity against DENV-2, only 14 per cent were immune in the 16 to 20 age group.
This partially explains the population’s susceptibility to explosive outbreaks and the high rate of dengue cases among young adults, the study’s authors said.
Population immunity against DENV-3 is lower than against DENV-2 in all age groups studied, and it is especially low in young people, dipping to 2.7 per cent for those aged 16 to 20 in the NEA study.
This serotype was last dominant in Singapore about three decades ago, but it has been dominant from January to April this year, said NEA.
A single housing block in Senja has become one of the most badly hit by Singapore’s worst dengue outbreak. Thirty-three residents are infected. Those living in the area say they have seen more fogging and inspections although some suspect the mosquitoes have been breeding not only inside homes, but elsewhere. CNA reports.
“The high base of dengue cases in the first few months of the year means a high ‘viral load’ within the population; this is a situation that is conducive for an outbreak once the other favourable conditions are aligned,” said NEA.
While NEA’s quarterly surveillance data showed that the proportion of DENV-3 cases had fallen while that of DENV-2 rose from April to June, there are more DENV-3 viruses circulating in Singapore than in the past.
“We would need to monitor the serotypes for a longer period to see a clearer trend, whether DENV-2 is back to dominant or there is going to be a shift to DENV-3,” said Assoc Prof Luo.
MORE MOSQUITOES, MORE PEOPLE WORKING FROM HOME
From May, a confluence of other factors pushed the numbers even higher.
The warmer and wetter weather as well as the increase in the mosquito population in many areas “carried the momentum of the high dengue case load of the first four months of the year over to the following months”, said NEA.
Between January and July this year, NEA detected about 13,800 mosquito breeding habitats islandwide. This is about 40 per cent higher than in the same period in 2019.
NEA’s Gravitrap surveillance system detected a 30 per cent increase in the Aedes aegypti mosquito population from May to June, compared to the February to March period.
There are still 391 active dengue clusters where about 600,000 households are located, with the largest clusters found around Aljunied Road/Geylang Road, Bukit Panjang Ring Road and Arthur Road near Katong.
Spike in dengue cases: Why Singapore may see worst outbreak in years
The sharp spike in case also coincided with the two-month COVID-19 “circuit breaker” period, said NEA.
“With more people staying at home, there would be more human hosts for the female Aedes aegypti mosquitoes to target, which is a day-biter and harbours within the indoor environment, and this would have partly contributed to the recent increase in cases,” said the agency.
Other factors at play during the circuit breaker include the reduction in some landscaping works due to manpower shortage and a pause in most construction activities which would have hampered good housekeeping of construction sites.
It is also possible that more cases of dengue were reported because of “better health-seeking behaviour” by the public who felt unwell or noticed symptoms during the COVID-19 pandemic, said NEA.
NEA STEPPING UP EFFORTS
The traditional dengue peak season lasts a few months, from May to October.
NEA is continuing its stepped up dengue inspection and outreach efforts. It conducted more than 552,000 inspections islandwide between January and July.
It is also working with partners to distribute educational materials and mosquito repellent to residents in dengue cluster areas.
Volunteers have been deployed every weekend since end-June to engage residents at large dengue cluster areas, reaching out to almost 55,000 people. These efforts will continue at other large dengue cluster areas over the coming weekends.
“We urge residents living in dengue cluster areas to protect themselves against mosquito bites, by doing the three simple steps – spray insecticide at dark corners, apply insect repellent, and wear long-sleeve tops and long pants,” said the CEO of NEA Tan Meng Dui.
“In our fight against dengue, both defensive and offensive actions are important. Such concerted individual and collective efforts are the most effective way to break the dengue transmission chain, and bring the dengue situation under control.”
NEA has developed checklist highlighting common mosquito breeding habitats. It is available for download at go.gov.sg/dengue-checklist.